Scientists at the University of Michigan Comprehensive Cancer Center have uncovered an important link between inflammation and breast cancer stem cells that suggests a new way to target cells that are resistant to current treatments.
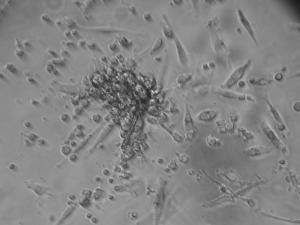
The researchers identified a receptor, CXCR1, on the cancer stem cells which triggers growth of stem cells in response to inflammation and tissue damage. A drug originally developed to prevent organ transplant rejection blocks this receptor, killing breast cancer stem cells and preventing their metastasis in mice, according to the study.
Cancer stem cells, the small number of cells that fuel a tumor's growth, are believed to be resistant to current chemotherapies and radiation treatment, which researchers say may be the reason cancer so often returns after treatment.
"Developing treatments to effectively target the cancer stem cell population is essential for improving outcomes. This work suggests a new strategy to target cancer stem cells that can be readily translated into the clinic," says senior study author Max S. Wicha, M.D., Distinguished Professor of Oncology and director of the U-M Comprehensive Cancer Center. Wicha was part of the team that first identified stem cells in breast cancer.
Results of the current study appear online Jan. 4 in the Journal of Clinical Investigation and will appear in the journal's February print issue.
CXCR1 is a receptor for Interleukin-8, or IL-8, a protein produced during chronic inflammation and tissue injury. When tumors are exposed to chemotherapy, the dying cells produce IL-8, which stimulates cancer stem cells to replicate. Addition of the drug repertaxin to chemotherapy specifically targets and kills breast cancer stem cells by blocking CXCR1.
Mice treated with repertaxin or the combination of repertaxin and chemotherapy had dramatically fewer cancer stem cells than those treated with chemotherapy alone. In addition, repertaxin-treated mice developed significantly fewer metastases than mice treated with chemotherapy alone.
"These studies suggest that important links between inflammation, tissue damage and breast cancer may be mediated by cancer stem cells. Furthermore, anti-inflammatory drugs such as repertaxin may provide a means of blocking these interactions, thereby targeting breast cancer stem cells," Wicha says.
Repertaxin has been tested in early phase clinical trials to prevent rejection after organ transplantation. In these studies, side effects seem to be minimal. There are no reports of using repertaxin to treat cancer.
Note to patients: This work was done in cell cultures and mice. Repertaxin is not available to patients at this time and no clinical trials are yet planned.
Breast cancer statisitics: 194,280 Americans will be diagnosed with breast cancer this year and 40,610 will die from the disease, according to the American Cancer Society.
Additional authors: Christophe Ginestier, Suling Liu, Mark Diebel, Hasan Korkaya, Ming Luo, Marty Brown, Jun-Lin Guan, Gabriela Dontu, all from U-M; and Julien Wicinski, Olivier Cabaud, Emmanuelle Charafe-Jauffret, Daniel Birnbaum, all from Universite de la Mediterranee, Marseille, France
Funding: National Institutes of Health, Breast Cancer Foundation, Taubman Institute, Department of Defense, Inserm, Institut Paoli-Calmettes, Institut National du Cancer, Ligue Nationale Contre le Cancer
Disclosure: The University of Michigan has filed for patent protection on this technology, and is currently looking for a commercialization partner to help bring the technology to market.
INTERNAL MEDICINE The internal medicine blog , where you can have details on alternatice medicine , latest trends in medicine , new drugs in the market , school of medicine etc
Blocking Inflammation Receptor Kills Breast Cancer Stem Cells, Study Finds
Sunday, February 28, 2010 at 6:23 PM Posted by Sajith
Major Improvements Made In Engineering Heart Repair Patches From Stem Cells
Friday, October 9, 2009 at 4:28 AM Posted by Sajith

University of Washington (UW) researchers have succeeded in engineering human tissue patches free of some problems that have stymied stem-cell repair for damaged hearts.The disk-shaped patches can be fabricated in sizes ranging from less than a millimeter to a half-inch in diameter. Until now, engineering tissue for heart repair has been hampered by cells dying at the transplant core, because nutrients and oxygen reached the edges of the patch but not the center. To make matters worse, the scaffolding materials to position the cells often proved to be harmful.
Heart tissue patches composed only of heart muscle cells couldn't grow big enough or survive long enough to take hold after they were implanted in rodents, the researchers noted in their article, published last month in the Proceedings of the National Academy of Sciences. The researchers decided to look at the possibility of building new tissue with supply lines for the oxygen and nutrients that living cells require.
The scientists testing this idea are from the UW Center for Cardiovascular Biology and the UW Institute for Stem Cell and Regenerative Medicine, under the guidance of senior author Dr. Charles "Chuck" Murry, professor of pathology and bioengineering. The lead author is Dr. Kelly R. Stevens, a UW doctoral student in bioengineering who came up with solutions to the problems observed in previous grafts. The study is part of a collaborative tissue engineering effort called BEAT (Biological Engineering of Allogeneic Tissue).
Stevens and her fellow researchers added two other types of cells to the heart muscle cell mixture. These were cells similar to those that line the inside of blood vessels and cells that provide the vessel's muscular support. All of the heart muscle cells were derived from embryonic stem cells, while the vascular cells were derived from embryonic stem cells or a variety of more mature sources such as the umbilical cord. The resulting cell mixture began forming a tissue containing tiny blood vessels.
"These were rudimentary blood vessel networks like those seen early in embryonic development," Murry said.
In contrast to the heart muscle cell-only tissue, which failed to survive transplantation and which remained apart from the rat's heart circulatory system, the pre-formed vessels in the mixed-cell tissue joined with the rat's heart circulatory system and delivered rat blood to the transplanted graft.
"The viability of the transplanted graft was remarkably improved," Murry observed. "We think the gain in viability is due to the ability for the tissue to form blood vessels."
Equally as exciting, the scientists observed that the patches of engineered tissue actively contracted. Moreover, these contractions could be electronically paced, up to what would translate to 120 beats per minute. Beyond that point, the tissue patch didn't relax fully and the contractions weakened. However, the average resting adult heart pulses about 70 beats per minute. This suggests that the engineered tissue could, within limits, theoretically keep pace with typical adult heart muscle, according to the study authors.
Another physical quality that made the mixed-cell tissue patches superior to heart muscle-cell patches was their mechanical stiffness, which more closely resembled human heart muscle. This was probably due to the addition of supporting cells, which created connective tissues. Passive stiffness allows the heart to fill properly with blood before it contracts.
When the researchers implanted these mixed celled, pre-vascularized tissue patches into rodents, the patches grew into cell grafts that were ten times larger than the too-small results from tissue composed of heart muscle cells only. The rodents were bred without an immune system that rejects tissue transplants.
Murry noted that these results have significance beyond their contribution to the ongoing search for ways to treat heart attack damage by regenerating heart tissue with stem cells.
The study findings, he observed, suggest that researchers consider including blood vessel-generating and vascular-supporting elements when designing human tissues for certain other types of regenerative therapies unrelated to heart disease.
One of the major obstacles still to be overcome is the likelihood that people's immune systems would reject the stem transplant unless they take medications for the rest of their lives to suppress this reaction. Murry hopes someday that scientists would be able to create new tissues from a person's own cells.
"Researchers can currently turn human skin cells back to stem cells, and then move them forward again into other types of cells, such as heart muscle and blood vessel cells," Murry said. "We hope this will allow us to build tissues that the body will recognize as 'self.'"
While the clinical application of tissues engineered from stem cells in treating hearts damaged from heart attacks or birth defects is still in the future, the researchers believe progress has been made. This study showed that researchers could create the first entirely human heart tissue patch from human embryonic cell-derived heart muscle cells, blood vessel lining cells and fiber-producing cells, and successfully engraft the tissue into an animal.
Future studies will try to move heart cell regeneration closer toward clinical usefulness, according to Murry and his research team. They forecast that such research would include testing other sources of human cells and developing techniques to create bigger patches for treating larger animals through surgical transplantation or through catheter delivered injections.
Lastly, they concluded, researchers would need to test whether tissue patches actually improve physical functioning after implantation in damaged hearts.
In addition to Stevens and Murry, the other researchers on this study, entitled Physiological Function and Transplantation of Scaffold-Free and Vascularized Human Cardiac Muscle Tissue, were Kareen L. Kreutziger, senior fellow in pathology; Sarah K. Dupras, research scientist in pathology; F. Steven Korte, senior fellow in bioengineering: Michael Regnier, associate professor of bioengineering; Veronica Muskheli, research scientist in pathology; Marilyn B. Nourse, postdoctoral scientist, Geron Corp.; Kira Bendixen, research technologist; and Hans Reinecke, research assistant professor of pathology.
The research was supported by grants from the National Institutes of Health, a Bioengineering Cardiovascular Training Grant, and a Pathology of Cardiovascular Disease Training Grant.
Stem Cells Transplanted From Marrow Into Heart May Improve Heart's Performance
Thursday, May 28, 2009 at 8:44 PM Posted by Sajith
The Cardiology department and the Area of Cell Therapy of Cordoba hospital Reina Sofia are carrying out clinical tests with patients who have suffered from a severe heart attack. With the implantation of the patient's stem cells, the heart regenerates thus improving its wall motion, that is, its cardiac performance. Indeed for the last four years, the Area of Cell Therapy of Cordoba hospital, led by haematologist Dr. Concha Herrera, has been implementing a therapy program with adult stem cells in patients with heart-related problems. However, this therapy is not a service the hospital offers yet. More specifically, at the end of 2007 the hospital ended a clinical test with patients who had suffered a severe myocardial infarction, that is, an obstruction of one of the main coronary arteries that stops the blood pump to the heart.
The test consisted of treating 30 people split into three groups of ten each at random. The first group was the control group, where patients received standard treatment for acute myocardial infarction; the second group was treated with stem cells directly implanted into the coronary artery affected using a catheterization; the third group was treated with a medicine called G-CSF, which makes cells move from the marrow to the blood, so that they get to the heart in a natural way, without having to do so through a catheter.
At the end of the test, the results revealed that the two groups treated without cells improved slightly, whereas patients transplanted with stem cells through the coronary arteries (vessels which bring the blood to the Herat muscle) did improve their ventricular function much more. This was interpreted as a significant decrease of the cardiac failure symptoms such as pain, fatigue and breathlessness when making small efforts.
Moreover, with this process it is possible to prevent some acute arrhythmias (change or irregularity in the rhythm of the heartbeat), which in many cases could result in the patient's death. ‘However, it does not prevent a future heart attack', Dr. Herrera assures.
In short, the stem cells transplanted from the marrow into the heart muscle have a double function: on the one hand they regenerate the heart cells, the cardiomiocites. In addition to this, they segregate a series of proangiogenic factors that produce blood vessels (angiogenesis) and can also produce the recruitment of stem cells that are in the myocardium itself.
The Are of Cell Therapy, led by Dr. Herrera, is currently developing other trials in the cardiology department, both in patients with acute myocardial infarction (35) and in those with chronic ischemic cardiopathy, due to one or more heart attacks suffered in the past, either months or years ago (20 patients). Moreover, in the last few months a new clinical trial has been started - so far in eight patients- who suffer from a disease called Dilated Myocardiopathy. The origin of this disease is unknown but it causes a very severe cardiac failure which conditions the need for a heart transplant in many cases. So far, ‘the results in these first patients are very satisfactory'.
'We will start shortly a clinical test where we will use stem cells from the marrow in diabetic patients who have the artery taking the blood to the lower limbs blocked. This pathology, called peripheral ischemia, can result in a limb being amputated'.
This work, published in Revista Española de Cardiología journal, has been awarded with a prize by the Sociedad Española de Cardiología.
Stem Cells And ABC Transporters Essential In Kidney Regeneration
Wednesday, February 18, 2009 at 3:06 AM Posted by Sajith

In a study funded by the Dutch Kidney Foundation (DKF) a research group at Radboud University Nijmegen Medical Centre in the Netherlands, found that stem cells and ABC transporter proteins are indispensable for tubular regeneration after acute kidney injury.Said project leader Dr. Rosalinde Masereeuw: 'To our surprise, our knockout mice for the ABC transporters P-gp and BCRP, P-gycoprotein and breast cancer resistance protein, were protected against acute kidney damage. This was the opposite of what we expected since the transporters usually have a protective function in excreting potentially toxic compounds, while these mice lack expression. Moreover, when we cross transplanted bone marrow between normal mice and the knockouts it turned out that bone marrow from the knockouts was the source of protection.'
Regeneration
Acute kidney injury is an important cause for the need of acute hemodialysis and a source of kidney failure. On the other hand, the kidney has a remarkable capacity for recovery. Stem cells seemed to have a limited share in the repair process, but now this study suggests otherwise.
'It was known that stem cells from the bone marrow express P-gp and BCRP abundantly but will downregulate them at differentiation. Repair of tubular damage in the kidney depends primarily on local cells but stem cells are involved as well. Further, we observed an upregulation in the expression of the transporters during ischemic injury. .So we thought they might be important in renal regeneration.'
Transporter Proteins
ABC transporters (ATP binding cassette transporters) form a superfamily of highly conserved transporter proteins whose functions are not yet well understood. However, BCRP and especially P-gp have been studied in more detail in man. These cell membrane pumps are responsible for the transport of many substances, for instance drug molecules in the intestine. P-gp plays an important role in drug resistance of tumour cells.
Masereeuw: 'Our new hypothesis claims a bigger role for bone marrow derived stem cells in kidney regeneration. A possible mechanism is the infiltration of macrophages. These large immune cells have subgroups one of which increases damage but another supports tissue regeneration.'
Also, the study showed that mice without P-gp expression lose renal tubular function in a way comparable to Fanconi syndrome in man. BCRP knockouts, on the other hand, have a normal kidney function.
Blocking P-gp and BCRP
There is a great need for novel therapies that limit kidney damage after acute injury by toxic substances or shortage of oxygen, as in transplant kidneys which have no blood supply during transport. The results from this DKF study are pointing at inhibition of the transporters in kidney or bone marrow to strengthen the regenerative power of stem cells.
'Next, we will try to discover the mechanism by which stem cells and ABC transporters contribute to kidney repair', concludes Dr. Masereeuw, 'and we will test the effect of transporter blockers in our mouse models. We are convinced there are good opportunities here for new drug targets.'
Don’t Go Changing: New Chemical Keeps Stem Cells Young
Wednesday, February 11, 2009 at 3:16 AM Posted by Sajith

Scientists at the Universities of Bath and Leeds have discovered a chemical that stops stem cells from turning into other cell types, allowing researchers to use these cells to develop new medical treatments more easily.
Stem cells have the ability to develop into many other cell types in the body, and scientists believe they have huge potential to treat diseases or injuries that don’t currently have a cure.
Professor Melanie Welham’s team at the University of Bath’s Department of Pharmacy & Pharmacology, collaborating with Professor Adam Nelson at the University of Leeds, have discovered a chemical that can be added to embryonic stem cells grown in the lab, allowing them to multiply without changing into other cell types.
This breakthrough will help scientists produce large stocks of cells that are needed for developing new medical therapies.
Professor Welham, who is co-director of the University of Bath’s Centre for Regenerative Medicine, explained: “Stem cells have great potential for treating spinal injuries and diseases like type I diabetes because they can change into a range of specialised cell types including nerve or pancreatic cells, which could be used to repair damaged tissues.
“Unfortunately, when you grow stem cells in the lab, they can spontaneously develop into specialised cells, making it difficult to grow large enough stocks to use for medical research.
“We’ve identified a chemical that will put this process on hold for several weeks so that we can grow large numbers of them in their unspecialised state. This is reversible, so when you take it away from the cells, they still have the ability to change into specialised cells.”
Professor Adam Nelson’s team, at the Astbury Centre for Structural Molecular Biology, made more than 50 chemical compounds that were tested for activity in the stem cells.The researchers found that the chemicals worked by blocking an enzyme, called GSK3, that can control when the stem cell switches to a more specialised cell type.
Professor Nelson, who is Director of the Astbury Centre at the University of Leeds, said: “This research is a great example of how small molecules can be used as tools to understand biological mechanisms.”
The research, supported by funding from the Biotechnology & Biological Sciences Research Council.
Brain Birth Defects Successfully Reversed Through Stem Cell Therapy
Tuesday, December 30, 2008 at 2:20 AM Posted by Sajith

Scientists at the Hebrew University of Jerusalem have succeeded in reversing brain birth defects in animal models, using stem cells to replace defective brain cells.
The work of Prof. Joseph Yanai and his associates at the Hebrew University-Hadassah Medical School was presented at the Tel Aviv Stem Cells Conference last spring and is expected to be presented and published nest year at the seventh annual meeting of the International Society for Stem Cell Research in Barcelona, Spain.
Involved in the project with Prof. Yanai are Prof. Tamir Ben-Hur, head of the Department of Neurology at the Hebrew University-Hadassah Medical School, and his group, as well as Prof. Ted Slotkin at Duke University in North Carolina, where Prof. Yanai is an adjunct professor.
Neural and behavioral birth defects, such as learning disabilities, are particularly difficult to treat, compared to defects with known cause factors such as Parkinson’s or Alzheimer’s disease, because the prenatal teratogen – the substances that cause the abnormalities -- act diffusely in the fetal brain, resulting in multiple defects.
Prof. Yanai and his associates were able to overcome this obstacle in laboratory tests with mice by using mouse embryonic neural stem cells. These cells migrate in the brain, search for the deficiency that caused the defect, and then differentiate into becoming the cells needed to repair the damage.
Generally speaking, stem cells may develop into any type of cell in the body, however at a certain point they begin to commit to a general function, such as neural stem cells, destined to play a role in the brain/ nervous system. At more advanced developmental stages, the neural stem cells take on an even more specific role as neural or glial (supporting) cells within the brain/ nervous system.
In the researchers’ animal model, they were able to reverse learning deficits in the offspring of pregnant mice who were exposed to organophosphate (a pesticide) and heroin. This was done by direct neural stem cell transplantation into the brains of the offspring. The recovery was almost one hundred percent, as proved in behavioral tests in which the treated animals improved to normal behavior and learning scores after the transplantation. On the molecular level, brain chemistry of the treated animals was also restored to normal.
The researchers went one step further. Puzzled by the stem cells’ ability to work even in those cases where most of them died out in the host brain, the scientists went on to discover that the neural stem cells succeed before they die in inducing the host brain itself to produce large number of stem cells which repair the damage. This discovery, finally settling a major question in stem cell research, evoked great interest and was published earlier this year in one of the leading journals in the field, Molecular Psychiatry.
The scientists are now in the midst of developing procedures for the least invasive method for administering the neural stem cells, which is probably via blood vessels, thus making the therapy practical and clinically feasible.
Normally, stem cells are derived from individuals genetically different from the patient to be transplanted, and therefore the efficacy of the treatment suffers from immunological rejection. For this reason, another important avenue of the ongoing study, toward the same goals, will be to eliminate the immunological rejection of the transplant, which will become possible by taking cells from the patient’s own body -- from a place where they are easily obtained -- by manipulating them to return to their stem cell phase of development, and then transplanting them into the patient’s brain via the blood stream. One important advantage of this approach will be to eliminate the controversial ethical issues involved in the use of embryo stem cells.
The research on the project has been supported by the US National Institutes of Health, the US-Israel Binational Science Foundation and the Israel anti-drug authorities.
Artificial Human Bone Marrow Created In A Test Tube
Monday, December 22, 2008 at 11:03 PM Posted by Sajith

This development could lead to simpler pharmaceutical drug testing, closer study of immune system defects and a continuous supply of blood for transfusions.
The substance grows on a 3-D scaffold that mimics the tissues supporting bone marrow in the body, said Nicholas Kotov, a professor in the U-M departments of Chemical Engineering; Materials Science and Engineering; and Biomedical Engineering.
The marrow is not made to be implanted in the body, like most 3-D biomedical scaffolds. It is designed to function in a test tube.
Kotov, principal investigator, is an author of a paper about the research currently published online in the journal Biomaterials. Joan Nichols, professor from the University of Texas Medical Branch, collaborated on many aspects of the project.
"This is the first successful artificial bone marrow," Kotov said. "It has two of the essential functions of bone marrow. It can replicate blood stem cells and produce B cells. The latter are the key immune cells producing antibodies that are important to fighting many diseases."
Blood stem cells give rise to blood as well as several other types of cells. B cells, a type of white blood cell, battle colds, bacterial infections, and other foreign or abnormal cells including some cancers.
Cancer-fighting chemotherapy drugs can strongly suppress bone marrow function, leaving the body more susceptible to infection. The new artificial marrow could allow researchers to test how a new drug at certain potencies would affect bone marrow function, Kotov said. This could assist in drug development and catch severe side effects before human drug trials.
Bone marrow is a complicated organ to replicate, Kotov said. Vital to the success of this new development is the three-dimensional scaffold on which the artificial marrow grows. This lattice had to have a high number of precisely-sized pores to stimulate cellular interaction.
The scaffolds are made out of a transparent polymer that nutrients can easily pass through. To create the scaffolds, scientists molded the polymer with tiny spheres ordered like billiard balls. Then, they dissolved the spheres to leave the perfect geometry of pores in the scaffold.
The scaffolds were then seeded with bone marrow stromal cells and osteoblasts, another type of bone marrow cell.
"The geometrical perfection of the polymer molded by spheres is very essential for reproducibility of the drug tests and evaluation of potential drug candidates," Kotov said. "The scaffold for this work had to be designed from scratch closely mimicking real bone marrow because there are no suitable commercially products.
"Certain stem cells that are essential for immunity and blood production are able to grow, divide and differentiate efficiently in these scaffolds due to the close similarity of the pores in the scaffold and the pores in actual bone marrow."
The researchers demonstrated that the artificial marrow gives a human-like response to an infectious New Caledonia/99/H1N1 flu virus. This is believed to be a first.
To determine whether the substance behaves like real bone marrow, the scientists implanted it in mice with immune deficiencies. The mice produced human immune cells and blood vessels grew through the substance.
Scientists Probe Limits Of 'Cancer Stem-cell Model'
Friday, December 19, 2008 at 4:32 AM Posted by Sajith

One of the most promising new ideas about the causes of cancer, known as the cancer stem-cell model, must be reassessed because it is based largely on evidence from a laboratory test that is surprisingly flawed when applied to some cancers, University of Michigan researchers have concluded.
By upgrading the lab test, the U-M scientists showed that melanoma---the deadliest form of skin cancer---does not follow the conventional cancer stem-cell model, as prior reports had suggested.
The findings, to be published as the cover article in the Dec. 4 edition of Nature, also raise questions about the model's application to other cancers, said Sean Morrison, director of the Center for Stem Cell Biology at the U-M Life Sciences Institute.
"I think the cancer stem-cell model will, in the end, hold up for some cancers," Morrison said. "But other cancers, like melanoma, probably won't follow a cancer stem-cell model at all. The field will have to be reassessed after more time is spent to optimize the methods used to detect cancer stem cells."
The cancer stem-cell model has steadily gained supporters over the last decade. It states that a handful of rogue stem cells drive the formation and growth of malignant tumors in many cancers. Proponents of the controversial idea have been pursuing new treatments that target these rare stem cells, instead of trying to kill every cancer cell in a patient's body.
But in a series of experiments involving human melanoma cells transplanted into mice, Morrison's team found that the tumor-forming cells aren't rare at all. They're quite common, in fact, but standard laboratory tests failed to detect most of them.
Scientists previously estimated that only one in 1 million melanoma cells has the ability to run wild, exhibiting the kind of unchecked proliferation that leads to new tumors. These aggressive interlopers are the cancer stem cells, according to backers of the model.
But after updating and improving the laboratory tests used to detect these aberrant cells, Morrison's team determined that at least one-quarter of melanoma cells are "tumorigenic," meaning they have the ability to form new tumors. The laboratory tests are known as assays.
"The assay on which the field is based misses most of the cancer cells that can proliferate to form tumors," Morrison said. "Our data suggest that it's not going to be possible to cure melanoma by targeting a small sub-population of cells."
Melanoma kills more than 8,000 Americans each year. The human melanoma cells used in the mouse experiments were provided---with the patients' consent---by a team from the U-M's Multidisciplinary Melanoma Program, one of the country's largest melanoma programs and part of the U-M Comprehensive Cancer Center.
"People were looking to the cancer stem-cell model as an exciting new source for the development of life-saving cures for advanced melanoma," said Dr. Timothy Johnson, director of the U-M melanoma program and a co-author of the Nature paper. "Unfortunately, our results show that melanoma does not strictly follow this model.
"So we'll need to redirect our scientific efforts and remain focused on the fundamental biological processes underlying the growth of melanomas in humans," said Johnson, a cutaneous oncologist. "And as we pursue new treatments for advanced melanoma, we'll have to consider that a high proportion of cancer cells may need to be killed."
Morrison and Johnson stressed that the team's findings do not broadly invalidate the cancer stem-cell model. Cancer stem cells likely do exist in some forms of cancer but are "probably much more common than people have been estimating," Morrison said.
The standard technique used to detect tumor-causing cancer cells in mouse transplants is called the NOD/SCID assay. NOD/SCID mice have defective immune systems. Scientists use the severely immunocompromised mice because the rodents don't reject transplanted human cancer cells the way normal mice would.
However, while the immune system in NOD/SCID mice is impaired, it's not completely inoperative. The mice lack T and B immune cells but still possess natural killer cells, which attack and destroy many of the transplanted human cancer cells.
Morrison's team replaced NOD/SCID mice with mice that lacked T cells, B cells and natural killer cells---and made a few other improvements to the assay. Using the modified assay, they found that about one in four transplanted melanoma cells formed tumors in the mice.
They concluded that previous studies using NOD/SCID mice vastly underestimated the number of tumor-causing melanoma cells, partly because natural killer cells wiped out many of the cancer cells. But once the natural killer cells were eliminated, the "more permissive conditions" allowed many of the transplanted melanoma cells to survive and thrive, the authors wrote.
Co-lead authors of the Nature paper are Life Sciences Institute research fellows Elsa Quintana and Mark Shackleton. In addition to Morrison and Johnson, other co-authors are U-M surgical oncologist Dr. Michael Sabel and U-M dermatopathologist Dr. Douglas Fullen.
The work was supported by the Howard Hughes Medical Institute, the Allen H. Blondy Research Fellowship and the Lewis and Lillian Becker gift.
Biologist Modifies Theory Of Cells' Engines
Monday, December 15, 2008 at 3:28 AM Posted by Sajith

Biologists have known for decades that cells use tiny molecular motors to move chromosomes, mitochondria, and many other organelles within the cell, but no one has been able to understand what "steers" these engines to their destinations. Now, researchers at the University of Rochester have shed new light on how cells accomplish this feat, and the results may eventually lead to new approaches to fighting pathogens and neurological diseases.
Michael Welte, associate professor of biology, shows in a paper published in the December 11 issue of Cell that the mechanisms that control the molecular motors are quite different from what biologists have previously believed. Before these findings, scientists assumed that the number of motors attached to an organelle determined how far and fast the organelle could travel, but Welte and colleagues have discovered that it is not the number of motors, but yet-to-be-discovered molecules that are likely the master regulators.
"The fact that motor number has nothing to do with regulating transport is extremely surprising, and somewhat unsettling to people working in vitro," says Welte. "It says we're really missing something when we study these motors only in the test tube instead of in a living cell."
Intracellular transport is crucial to a cell's health, says Welte. For instance, during cell division, one copy of each of the cell's chromosomes migrates to one side of the cell while the other copy moves to the other side. If this movement is disturbed, it could cause an imbalance of chromosomes in the daughter cells, which might die or become cancerous. Similarly, neurons, some of which are as much as three feet in length, manufacture proteins and organelles at one end and then must move that precious cargo all the way to the far end where they'll be used. This is an enormous task, says Welte, and defects in this transport are thought to cause a number of neurological diseases.
Given the difficulty of investigating these tiny motors acting within the cell, biologists have performed basic experiments on them outside of the cell in a carefully controlled environment. This led them to believe that the speed and distance an organelle could be transported depended on how many motors were pulling it, says Welte. Thus, the scientists reasoned, perhaps the cell simply attaches the right number of motors to an organelle to send it the right distance. Although this "multi-motor" hypothesis is very simple and elegant, says Welte, whether it actually holds true within living cells had never been tested.
Welte's graduate student, Susan Tran, decided to perform that test. She created fruit-fly eggs lacking a type of molecular motor called kinesin and found that certain organelles stopped moving—strong evidence that kinesin is responsible for their transport. Tran then made another type of mutant eggs, this time ones that produced only about half the number of kinesin motors of a regular egg. In both types of eggs, organelles were transported with the same speed and the same distance.
Welte needed to know if this equality was because the normal egg was simply utilizing only half the available kinesin motors, or if some master regulator was controlling the organelle's progress, regardless of the number of motors moving it. To do this, Welte turned to Steven Gross, associate professor of developmental and cell biology at the University of California. Gross' group uses an apparatus called "optical tweezers" that employs laser light to measure the tiny forces the motors generate. The team found that organelles in regular cells are pulled with twice the force of Tran's mutant, low-kinesin cells.
"That clinched it for us," says Welte. "Yes, there are multiple motors moving organelles around, but exactly how many doesn't matter. There is something else in the cell that's controlling all the motors. That opens up a big area for research—find what's driving these motors and maybe we can control them all by controlling one thing."
Welte and his team are now looking at where in the cell this signal comes from and how it influence the motors. Although Welte's team studied fruit fly eggs, the motors moving the organelles are present in all animals and employed for many tasks, including transport in human neurons.
Welte also points out that viruses, including HIV, make use of the same kind of motors to move about the cell, first to get from the site of penetration to the nucleus, where they multiply, and then to get progeny viruses back to the cell surface. If Welte and others can figure out how cells normally control these motors, it may be possible to prevent HIV from taking control of the motors and thus to keep it, and other intracellular pathogens, at the edge of the cell where they can do little harm.
This research was funded by the National Institutes of Health, and includes researchers from the University of Rochester, the University of California Irvine, and University of Texas at Austin
Search
Labels
- Alzheimer's (10)
- Antibiotics (7)
- Anxiety (1)
- articles (2)
- Bacteria (1)
- behavioral abnormality (1)
- Bio technology (1)
- Brain (8)
- breast cancer (6)
- Cancer (40)
- cancer treatment (7)
- chemotherapy (6)
- Chlamydia (1)
- Cytology (3)
- Death (1)
- Diabetes Mellitus (7)
- Diet (17)
- DNA (1)
- Doctors (1)
- epilepsy (2)
- Fossil (1)
- fruits (1)
- genes (6)
- Genetics (13)
- Geriatrics (1)
- Health (12)
- Heart diseases (9)
- Herbal Medicine (2)
- HIV and AIDS (7)
- influenza (1)
- Inventions (1)
- IVF (1)
- latest findings (1)
- Life style (2)
- Lung Cancer (1)
- Lung Disease (9)
- Microbiology (1)
- Multiple Sclerosis (1)
- Nanotechnology (3)
- Neonatology (1)
- neurology (1)
- News (18)
- Parkinsonism (2)
- Prevention (1)
- Primates (1)
- Prostate cancer (1)
- Prosthetics (1)
- seizure (2)
- Skin (1)
- STD (2)
- Stem cells (9)
- Stroke (1)
- Surgery (2)
- Swine flu (11)
- Virus (1)
- weight loss (1)
Search The Web
Minyx v2.0 template es un theme creado por Spiga. | Minyx Blogger Template distributed by eBlog Templates
